PhilHealth boosts benefit packages for heart diseases by over 1600%

MANILA, Philippines — The Philippine Health Insurance Corp. (PhilHealth) ramped up the coverage of its benefit packages for heart diseases by as much as 1,629%.
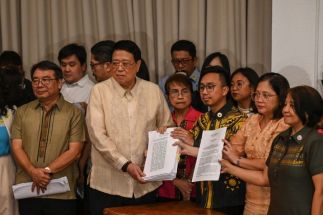
PhilHealth announced the enhanced benefit packages on Thursday, January 2, as detailed in Circular 2024-0032 issued on Dec. 21, 2024.
For inpatient admissions, Filipinos with ischemic heart disease — a condition caused by reduced blood flow to the heart — and acute myocardial infarction, or heart attacks, can now avail of increased coverage under two enhanced benefit packages.
The reimbursement rate for percutaneous coronary intervention, a non-surgical procedure to clear blocked arteries and remove plaque buildup, has been raised to P523,853 — about 17 times higher than the previous coverage of P30,300.
Patients may avail of this procedure at any of the 70 accredited cath labs in the country.
The second enhanced package covers fibrinolysis, a treatment for dissolving blood clots. It now has a case rate of P133,500, or a 341% increase from the previous amount of P30,290.
The state insurer also increased the benefit package for emergency medical services with coordinated referral and interfacility transfers to P21,900 and cardiac rehabilitation to P66,140.
The total value of the benefit packages covers both the payment to the healthcare institution and the fees for healthcare professionals.
The benefit packages also cover services such as emergency care, medications, laboratory tests, medical supplies, equipment, and other administrative fees.
They will apply to accredited public and private health facilities classified as Levels 1 to 3, equipped to provide the necessary medical treatments and procedures. The levels correspond to the range of services each hospital can offer.
PhilHealth President Emmanuel Ledesma Jr. said they worked with partner health facilities to adjust reimbursement rates for heart diseases.
They hope this will assist patients, including those who suffered from heart disease during the 2024 holiday season, following a reported rise in cases by the Department of Health (DOH).
RELATED: Holiday Surge: 91 new stroke cases in a week, heart and lung conditions rise
Ledesma stressed that "there should be no co-payment for inpatient admissions in both public and private hospitals," meaning members should not pay additional out-of-pocket costs for their hospital stay.
He also urged Filipinos to take advantage of the Konsulta care benefits, which centers on outpatient services to prevent chronic illnesses and complications through early detection, while ensuring accessible healthcare.
The Konsulta services include consultation, health risk screening and assessment, selected laboratory and diagnostic tests, and affordable medications.
Operating on zero government subsidy
PhilHealth is expanding its benefit packages without any government subsidy for 2025. It will run with the approved P284-billion corporate operating budget, mainly sourced from premium contributions, for 2025.
The government explained its decision to withhold funds from PhilHealth, saying that its reserve fund of around P600 billion is enough to reduce contributions and increase case rates.
The state insurer has been raising case rates in 2024 following pressure from Congress during the 2025 budget hearings.
Civil society groups, health advocates and finance experts criticized the P74-billion budget cut, arguing that defunding PhilHealth does not solve the issue of health financing.
Concerns over a potential increase in contributions were also raised, but PhilHealth assured the House of Representatives during a Dec. 17, 2024 hearing that it will reduce contributions to 3.25% of members' earnings, down from the current 5%.
- Latest
- Trending