P137.6 billion in benefits paid this year – PhilHealth

MANILA, Philippines — The Philippine Health Insurance Corp. (PhilHealth) paid a total of P137.6 billion in benefit claims to more than 12,000 accredited health care facilities nationwide this year.
The payment, made from Jan. 1 to Oct. 31, was P37.6 billion or 37.7 percent higher than the P99.9 billion posted in the same period last year.
The national average turnaround time for claims processing also significantly improved to 25 days from the 60 days prescribed under Republic Act No. 10606 or the National Health Insurance Act of 2013.
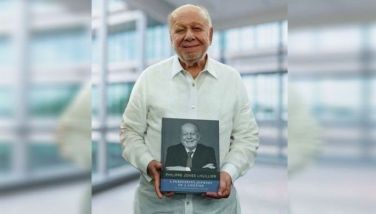
“The reduced turnaround time has been commended by partner hospitals around the country. It is helping them maintain liquidity, ensuring steady supply of medicines, salaries for health workers and continuous improvement of facilities which all translate to better services to members,” PhilHealth president and CEO Emmanuel Ledesma said in a statement.
He urged health care facilities to invest in adequate and properly-trained human resources to ensure the submission of “good” claims within the prescribed filing period.
“This will help ensure claims are complete and in order, free from deficiencies, incomplete documents or signatures and unreadable attachments, among other reasons,” he said.
Claims are returned to the hospitals if there are discrepancies in entries; incomplete, inconsistent or unreadable documents and improperly completed claim forms.
Claims are denied payment due to late filing/re-filing, non-compensable cases and if confinement happened when the hospital has accreditation issues.
“The strict review and adjudication of claims is in keeping with PhilHealth’s fiduciary responsibility to our members. This is helping us ensure that the funds entrusted to us by the Filipino people are spent judiciously and responsibly,” Ledesma stressed.
“We are reaching out to the hospitals around the country to inform and educate them on the latest claims policies, guidelines and pertinent requirements,” PhilHealth said.
Ledesma also said they are currently exploring the possibility of adopting artificial intelligence (AI) for claims processing.
“We have just completed a study conducted by experts on how AI can aid us in receiving and processing claims at break-neck speeds never before seen,” Ledesma said. “We are confident that with the support of our health care partners, this will happen in the very near future.”
- Latest
- Trending