Vaccine 101: Is there such a thing as the 'right vaccine' for me?

With more and more vaccines being granted an Emergency Use Approval from the Philippine Food and Drug Administration, people are wondering what vaccine is right for them. This is a good start, and a step in the right direction. But based on the recent survey of the SWS on vaccine hesitancy, there are still a lot of people scared of the vaccine. Lots of people are saying that it was produced too quickly. Others are wondering if COVID-19 is even real.
This is why I invited Dr. Benjamin Co of the Pharmacy and Therapeutics Committee of Cardinal Santos Hospital to clarify some questions on a recent episode of Pamilya Talk.
Why vaccines were developed so fast
Dr. Co agreed that the development of the COVID-19 vaccine is really fast, but he clarified that the platforms that the vaccines came from have been tried and tested. Like the methods needed to make inactivated vaccines have been in use for many years — as with the polio vaccine, hepatitis A, rabies, etc. It wasn't therefore that difficult to apply these platforms and create an inactivated COVID-19 vaccine.
Dr. Co stressed that the different phases needed to develop vaccines are in fact the same phases in the development of any medicine. All vaccines have gone through pre-clinical testing, either on animals or on cell lines, to establish if it produces an immune response, such as the production of antibodies. Secondly, it must be established that the immunological response is safe. Following this, the first stage of human clinical trials can start.
At the end of the day, the medical community and the drug developers are all looking at one endpoint: the safety of the medication.
So the quickness of the vaccine development isn't an issue here, since every COVID-19 vaccine has undergone the necessary trials to ensure its safety and efficacy. Combining the different phases of development allows us to see the data immediately, and this is done with various drug developments such as in chemotherapy.
How the vaccines work
Now the question is, how do the different vaccines work?
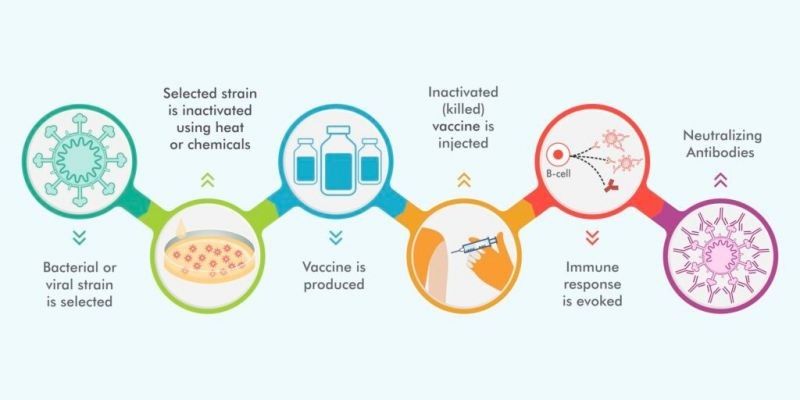
- First, according to Dr. Co, you have the inactivated vaccines, which uses the dead virus to stimulate an immune response. This is a technique being used to develop vaccines for polio, Hepatitis A, rotavirus, and so on, and is a tried and tested method of safe and effective vaccination. Examples of an inactivated vaccine are Sinovac's CoronaVac, as well as Bharat Biotech's Covaxin, which recently received its EUA from the FDA.
- Next you have protein-based vaccines, which use fragments and pieces of the virus to stimulate immune response. The EU Commission recently announced that it may eventually expand its portfolio of COVID-19 jabs to protein-based vaccines such as those currently being developed by Novavax and Sanofi/Glaxo-Smith-Kline—the latter of which is being delayed until the end of 2021 after their interim results showed a low immune response in older adults.
- Furthermore, there are what are known as mRNA or DNA vaccines, which use the virus' genes to stimulate immune response. According to the Center for Disease Control (CDC), these are new types of vaccines to protect against infectious diseases that teach our cells how to make a protein, or even just a piece of a protein, that triggers an immune response.
- Finally, the fourth type of vaccine that is in use for COVID-19 is the viral vector vaccine, which use a modified version of a different virus (known as the vector), to deliver important instructions to our cells. It works in much the same way as an mRNA vaccine in that it gives our cells instructions on producing an immune response via the production of a spike protein. The Johnson & Johnson vaccine is an example of a viral vector vaccine, and while it has been known to cause blood clots in a small amount of the population, the rollout has been resumed in the US. Women under the age of 50 however are cautioned that the risk of rare blood clots with low platelets after vaccination is a possibility, as per the CDC.
The right vaccine for you
We polled our online audience, and the Pfizer vaccine came out as frontrunner, followed closely by Sinovac’s CoronaVac. Dr. Co was quick to dispel any false hopes of Pfizer being rolled out by the LGUs, saying “it will never be available in the Philippines."

This is likely in part to the ultra-cold-chain requirements needed for Pfizer to be rolled out, as well as the extreme shortage of this particular brand of vaccine due to the developed countries having sewn up most of the doses for their own people. Compare this for example with Sinovac or even Bharat Biotech’s Covaxin, which has increased the production of their vaccine to answer the global call for vaccines.
Dr. Co reminded us that all the vaccines that have been granted an EUA in the Philippines have undergone exhaustive trials and have been proven to be safe for emergency use.
Most important of all, the best vaccine is the one that is immediately available to you. Based on research, all vaccines that have been granted an EUA have shown efficacy against severe COVID-19 cases, which is what is needed in the first line of defense against new and virulent diseases.
Furthermore, there is a global shortage of vaccines. So if you are able to get vaccinated, then by all means, you should take the opportunity to do so!
--
Please watch Pamilya Talk on Facebook, YouTube and Kumu (@JingCastaneda – 6 p.m. Monday and Wednesday; 7 p.m. Tuesday). Please share your stories or suggest topics at jingcastaneda21@gmail.com. You can also follow and send your comments via my social media accounts: Instagram, Facebook, YouTube, Twitter and Kumu.



















